If you’re in treatment or pregnant and you need to speak to a nurse urgently during this time then please ring 0114 271 1900 and ask for the ACU nurse on call.
We are delighted that most of our services are now back up and running. We have put many measures in place to make sure that when you have your treatment at Jessop Fertility you and our staff will be as safe as possible.
We know that in the current circumstances you may appreciate some extra emotional support and, as one of our patients, you can access this free of charge – please just contact us on 0114 2268050 to make an appointment with one of our specialist counsellors.
If you would like any further information about Covid-19 and fertility treatment, please have a look at the HFEA website at www.hfea.gov.uk
Why families choose us
As one of the leading UK hospital based fertility centres, you can be confident that we will do all we can to give you the very best chance of becoming a parent. You will have access to the very latest treatments provided by our expert fertility team who have a track record of excellent success rates. We will tailor our care to you as individuals and will spend time discussing the right treatment(s) after carefully reviewing your needs.
Stefanie Maddocks
Thanks to the wonderful team at Jessop fertility we have a beautiful little daughter who celebrated her 2nd birthday last month. Every member of staff that we have met on our fertility journey was so kind and supportive and we will be forever grateful.
Tanya Stack
The staff were fantastic through our journey, empathetic, kind and friendly. they helped keep us positive but realistic and we were treated as an individual couple, not just another patient. treatments are really tailored to your needs.
Lindsay Coupe
We couldn’t have been any happier after the treatment we received resulted in our little miracle Harper Jessops were amazing from start to finish, personal, friendly, kind and caring during every step, especially ringing to tell me the fabulous news on my birthday. I would highly recommend Jessops and do frequently. Thank you from the bottom of our hearts xxx.
Tara Chappell
We have a beautiful daughter who is here thanks to the amazing work of Jessops. The IVF process is gruelling but we were well supported and given great advice about next steps during the process. My enduring memory of Jessops is the scan where the staff were almost as delighted as I was to learn we were pregnant.It truly felt that staff were fighting with you for things to work. We would recommend without reservations to anyone considering starting on the complex journey of IVF.
Emma Sarah Whelan
The staff are so friendly and give amazing support I had 2 failed attempts of icsi before 1 of 2 frozen embryos worked they gave me and my other half the little girl we had always wanted they give us the opportunity to be parents and now my 5lb 6oz who was born 22 December 2016 is now nearly 2 years old and it’s all thanks to jessops fertility and We will be forever grateful thank you jessops fertility
Jane Kilburn
We have an amazing daughter who is nearly 2 and wouldn’t be here without Jessop Fertility. The care we received at every stage of IVF was fantastic and all the staff were wonderful. After 8 long years they made our dreams come true and we can’t thank them enough
Laura Gregory
We have 2 wonderful children who are only here due to the wonderful staff at Jessops. The love, care and expertise is second to none. Jessops will always hold a special place in our hearts and we cannot thank them enough!
Rebecca Cottam
We have a beautiful daughter and it’s all down to the staff at Jessops fertility. From start to finish, they were kind and considerate and showed a genuine care towards our little family.
Sperm and Egg Donation
Donor sperm is used to treat couples where the man is unable to produce sperm, or because of abnormalities in his sperm. It is also used to treat single women and women in same-sex relationships who wish to have a child. Donor eggs are used by women who are unable to produce their own eggs.
Become a Sperm Donor Become an Egg DonorOur Services
Jessop Fertility has already helped thousands of men and women become parents and has experience of successfully treating even the most complex infertility cases using advanced techniques and a personalised approach.
Our world-renowned fertility experts have excellent pregnancy and live birth rates and are committed to finding the right treatment options available to you.
Download our brochures:
Guide to Services Preconception adviceWhat is Egg Freezing?
Egg freezing is a service available for women who hope to try to have a baby in the future and are worried about declining fertility. Women’s fertility decreases with age because the quality and number of eggs are reduced which makes the chance of conceiving naturally harder. Egg freezing involves collecting the eggs, freezing and storing them to be used when you are ready in a fertility treatment.
Is Egg Freezing for me?
If you are worried about your fertility and not ready to have a child or you haven’t found the right partner you might want to consider egg freezing.
What does egg freezing involve?
The first stage of the process is to arrange a fertility health check (link to this – see item below) then you proceed onto the following.
Medical Consultation
During the consultation a doctor will talk through your medical history and the results of your tests. They will discuss the egg freezing procedure in detail and if you are suitable to proceed.
Counselling
Counselling with one of our fertility counsellors is part of the process. This will provide you with the opportunity to explore the implications of any decisions/course of action you wish to consider. You can talk to one the Counsellors before, during and after treatment.
Nurse Appointment
At this appointment you will be tested for any infectious diseases (HIV, Hepatitis B & C), taught to self-inject the hormone drugs and ask any questions you have regarding the treatment plan. We are unable to offer treatment if you are HIV or Hepatitis B or C positive.
Egg retrieval
You will commence treatment on day 2 of your menstrual cycle and the whole process takes approximately two weeks. Regular monitoring appointments will be arranged until you are ready for egg collection. On the day of egg collection your procedure will be under local anaesthetic with pain relief medicines. You will be discharged home the same day. It is advisable to arrange to be collected by a relative or friend.
What are the chances of the frozen eggs being used successfully in future treatment?
Currently we do not have data for success rates for this Unit, as the service has only recently become available. From worldwide experience, we know that about 50-70% of eggs will survive the freezing and thawing process.
It is important to note that there can be no guarantees that any of the frozen eggs will result in healthy embryos suitable for treatment or a successful pregnancy.
Costs
The clinic has an open and transparent pricing system (link) The cost of egg freezing includes 5 years storage costs. After this time, we will contact you annually to ask if you wish to continue to store these (there will be additional cost to storage beyond 5 years)
Who shall I contact if I would like more information?
If you think egg freezing may be an option for you, please contact us on 0114 226 8050 and we will answer any questions you may have or you can book an appointment.
Why get a fertility health check?
Men and women request fertility health checks for various reasons. By discussing your health, medical history and lifestyle along with completing a few simple fertility tests, we can assess your fertility health and give you general reassurance or advice regarding your fertility results.
Do I need to be referred?
No you can self-refer. Contact the Unit on 0114 226 8050 and request an appointment.
Who are fertility health checks for?
We offer fertility health checks for males, females and couples.
What is included?
For a fertility health check you will be given an appointment with a specialist nurse. During the consultation you will:
Female:
- Discuss your medical history, focusing on areas that could impact on your fertility health and how to improve them.
- Undergo a blood test called AMH, which will assess the amount of egg stores in your ovaries
- Receive an internal ultrasound scan to assess the ovaries and uterus to detect any abnormalities and look at the potential of the ovaries to produce eggs.
Male:
- Discuss your medical history, focusing on areas that could impact on your fertility health and how to improve themM
- Arrangements will be made for you to attend Andrology services for a Semen Analysis
What happens next?
Once all your results are collated and reviewed, the nurse specialist will arrange a time to contact you to discuss the test results. If the health check has highlighted any concerns they will also discussed. The results will be summarised in a written report.
How much do the health checks cost?
We offer an open and transparent pricing system, with a fixed cost for males, females and couples.
As part of the fertility health assessment other tests will be discussed. The additional tests may be undertaken by your GP. However, you may choose to have the additional test during your assessment, these will incur individual costs.
It is important to understand that the fertility health check results do not guarantee a pregnancy.
In Vitro Fertilisation (IVF) is a treatment used for couples with, for example, mild sperm defect, or tubal infertility.
IVF is the medical term for the ‘test tube baby' technique. The principle of IVF treatment is for us to stimulate your ovaries with hormone medication. The additional hormones encourages the development of several eggs (usually between 6 to 10) rather than the one or two eggs that you would normally produce. This process takes about two weeks.
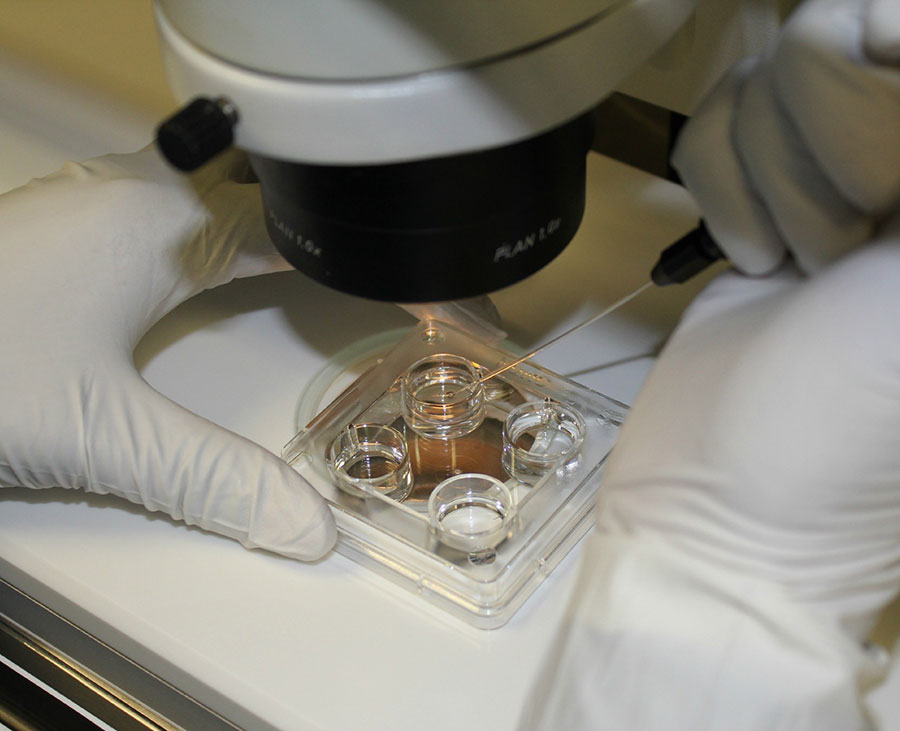
The eggs are removed from your ovaries by passing a needle into the follicle in the ovary to find the eggs. This is a simple procedure performed under mild sedation and local anaesthetic. Once the eggs have been collected they are placed with the sperm in a plastic dish and incubated overnight. The following morning the embryologist checks for fertilisation. The fertilised eggs are now called embryos and are allowed to develop for another one to four days. One or two good quality embryos are selected for transfer (on day 2, 3, 4 or 5 after fertilisation). These embryos are then placed into the uterus using a very soft plastic tube called an embryo transfer catheter. This is a simple procedure that does not require an anaesthetic.
Single Embryo/Blastocyst transfer:
Couples who are below 37 years of age and are on their first (and possibly subsequent cycles), generally have a higher chance of a pregnancy but are at a higher risk of a multiple pregnancy (twins or more).
If you fall into this patient group then we will recommend that you have a single embryo transferred. This will be performed at the blastocyst stage (day 5 after egg collection) if possible, but can also be done earlier after 2 or 3 days. Transferring embryos at day 5 gives us more information about them and allows us better selection of the best embryo. All other good quality embryos may be frozen and stored for further treatment.
Blastocyst transfer is not suitable for every patient although all of our patients are encouraged to have blastocyst transfer if possible - please ask your embryologist for advice.
We do not charge extra for this service.
Intra Cytoplasmic Sperm Injection (ICSI) is a process that works alongside IVF. We use ICSI when the sperm concentration or motility (percentage of sperm swimming) is too low for us to do conventional IVF.
ICSI is used in conjunction with IVF if there is a severe problem with the sperm. The ICSI procedure is the direct injection of single sperm into each mature egg. ICSI is a process we also provide for couples when we retrieve sperm surgically from the male partner.
Single Embryo/Blastocyst transfer:
Couples who are below 37 years of age and are on their first (and possibly subsequent cycles), generally have a higher chance of a pregnancy but are at a higher risk of a multiple pregnancy (twins or more).
If you fall into this patient group then we will recommend that you have a single embryo transferred. This will be performed at the blastocyst stage (day 5 after egg collection) if possible, but can also be done earlier after 2 or 3 days. Transferring embryos at day 5 gives us more information about them and allows us better selection of the best embryo(s). All other good quality embryos may be frozen and stored for further treatment.
Blastocyst transfer is not be suitable for every patient although all are encouraged to have if if possible - please ask your embryologist for advice.
We do not charge extra for blastocyst transfer.
Egg sharing is when a woman donates half of her eggs to another woman and receives her treatment at a reduced cost. Not all women are suitable to be egg share providers; there are strict criteria to be met, and a range of specific issues to consider. Counselling plays a vital role in this decision making process and is essential for all egg share providers and egg recipients
Frozen Embryo Replacement (FER) is an option for patients who have embryos frozen from a previous treatment.
IVF treatment may result in 'spare' embryos. We are able to offer freezing of these embryos to allow you to use them in a FER cycle. Stimulation drugs are not always administered for this treatment; careful monitoring is carried out to time your ovulation perfectly. Which allows us to calculate when the lining of the womb will be suitable for your embryo(s) to implant and at this stage we will arrange for your embryo transfer. The embryo is placed into your uterus using a very soft plastic tube called an embryo transfer catheter. This is a simple procedure that does not require an anaesthetic.
Surgical Sperm Recovery is an option for patients who do not produce sperm in their ejaculate or where ejaculation is not possible
Surgical Sperm Recovery is the process of sperm samples being obtained directly from the testicle by this simple procedure, which is usually performed under mild sedation and local anaesthetic. Sperm are extracted using a very fine needle. The main reasons for this procedure are the absence of the tubes carrying the sperm, blockage of the tubes, a vasectomy or other testicular disorders.
Sperm Sharing is also an option available to those couples willing to both donate and be recipients
In sperm share a man becomes a sperm donor for other patients and receives his treatment at a reduced cost. Not all men are suitable to be sperm sharers; there are strict criteria to be met, and a range of specific issues to consider. Counselling plays a vital role in this decision making process and is essential for all sperm sharers and their partners.
This treatment is used for couples with unexplained infertility or for women with problems with ovulation.
The principle of SIUI is to stimulate the ovaries with hormone medication so that one or more eggs are produced. The man's semen (either from a partner or a sperm donor) is prepared to separate out the high quality sperm. This is then inseminated high up into the uterus with a soft catheter. Fertilisation of the eggs can then occur naturally.
Occasionally, couples may be advised to have intercourse rather than the insemination. We will take blood samples and scan your ovaries to make sure your IUI is timed to coincide with ovulation, which will maximise your chances.
Egg Donation is used when there is an issue with the female's eggs
Egg Donation is a treatment that involves the use of eggs provided by a donor. Occasionally, a patient may be treated with eggs from a donor who is already known to them. The eggs are fertilised with your partner´s sperm to allow their use in an FER cycle. This treatment may benefit couples that cannot conceive because the female does not produce her own eggs due to premature ovarian failure, removal or absence of the ovaries, a genetic disorder, disease, or sometimes in older women the eggs may be of poorer quality.
Donor Insemination (DI) is a treatment used when there are serious issues with the quality of the man's sperm. We also use it to treat single women and women in same-sex relationships.
Donor Insemination (DI) involves the use of sperm from a donor.
Stimulation drugs are not always required for this treatment; careful monitoring is carried out to ensure the correct time for insemination.
The sperm sample is prepared and then a soft plastic tube (catheter) is used to place them into your uterus.
We’re licensed by the HFEA to freeze and store eggs, embryos and sperm.
We use a super-cooling technique for egg and embryo freezing called vitrification, which gives us consistently high survival rates.
We can help diagnose fertility conditions using ultrasound scans and appropriate blood tests. Investigations can look at ovulation and the way the dominant egg-containing follicle develops.
Your GP may refer you to a specialist centre (e.g the Andrology Department in the Jessop Wing) to have tests performed on the semen sample.
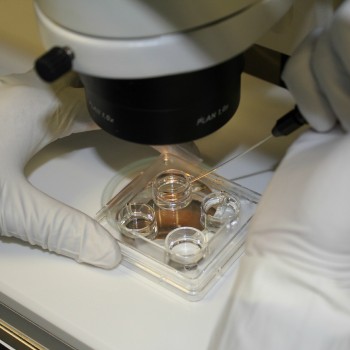
If you have been referred for a semen analysis this will involve producing a semen sample (usually by masturbation) in the Andrology department. The semen sample is then observed down the microscope in order to assess the quality of the sperm.
A general observation is made about the seminal fluid and then several observations are made on the sperm themselves. We look at the motility (how the sperm move around in a sample), the concentration (the sperm count) and normal forms (the number of 'normal' sperm). All of this information will be sent to your referring doctor for discussion with you and your partner. The information is also used if you require fertility treatment and a decision can made about what type of treatment is suitable for you.
A trial sperm preparation is a basic semen analysis test to check the ‘quality’ of your sperm and suitability for treatment.
One of the most challenging decisions for an embryologist is deciding which of your embryos gives the best chance of a successful pregnancy. Jessop Fertility has introduced the latest technology to help us do this. We have invested in two types of time lapse technology: Primovision™ and Embryoscope™.
Cameras located within incubators take images of your embryos approximately every 10 minutes without them ever having to leave the incubator. This gives us videos of the embryos’ development and allows us to identify which ones are most likely to lead to a successful pregnancy.
We aim to use time lapse for the vast majority of our patients. This technology is part of your treatment and there will be no extra charge.
Embryo transfer is one of the most sensitive and critical procedures in IVF treatment. EmbryoGlue™ is a medium developed exclusively for embryo transfer and can have an implantation-enhancing effect. It is uniquely developed to mimic the conditions in the female uterus in order to help embryos implant after transfer.
All our patients receive EmbryoGlue™ as part of the package. There is no extra charge for this.
Jessop Fertility now provides Preimplantation Genetic Testing (PGT) which allows our embryologists to identify embryos that have the incorrect number of chromosomes at a very early stage to avoid transferring them to the uterus. During this procedure some cells from the embryo are assessed to see if there are any chromosomal abnormalities.
Using only those embryos that do not have chromosomal abnormalities can increase the chances of IVF being successful as we can chose embryo(s) for transfer that will be much more likely to implant and create a healthy pregnancy. It can also reduce the chance of a miscarriage.
This service is only appropriate for certain patients and our doctors will discuss this with you if they feel that it would increase your chances of a successful pregnancy.
PGS (preimplantation genetic screening) can be used to determine if embryos created after IVF have normal chromosomes. Embryos with abnormal chromosomes might look and develop normally but may be more likely to result in a miscarriage or the birth of a child with, e.g. Down Syndrome.
PGD (preimplantation genetic diagnosis) can be used to screen for a particular genetic predisposition to a genetic disorder (i.e. if there is a genetic condition that runs in the family). At the moment we provide this service in collaboration with Guy’s Hospital in London.
In PGS and PGD a small number of cells are removed from the embryos. The embryos are then frozen and the cells sent to specialist labs for analysis. Unaffected embryos can then be thawed and transferred back into the uterus at a later date.
Endometrial scratch research no longer supports offering this procedure to our patients.
Jessop fertility’s own Mr Metwally was the Chief Investigator for a large national multi-centred randomised control trial to provide conclusive evidence if the procedure of Endometrial Scratch improved pregnancy outcomes for patients undergoing their first cycle of IVF/ICSI. The study was conducted in Sheffield and 15 other sites in the UK recruiting over 1000 patients over 2.5 years. Half of the patients were randomised to treatment as usual and the other half had the endometrial scratch 7-10 days prior to starting their treatment. Results showed there was no statistical difference in live birth rate in either group. Furthermore secondary outcomes of clinical pregnancy rate, embryo implantation rate and obstetric complications showed no difference between both groups of patients.
This is further supported by a study of Endometrial scratch in patients having their second or subsequent cycle of IVF/ICSI, conducted by Lensen et al across 5 countries also demonstrated that the endometrial scratch has no beneficial effect on the outcome of IVF/ICSI.
Why should I think about banking my sperm before I have my vasectomy?
A vasectomy is a long term (and usually permanent) form of birth control. However, some men may change their mind after their vasectomy and decide that they would like to have more children. Banking sperm is a safe and cost-effective way of providing a chance to do this after a vasectomy.
How do I arrange for sperm banking?
Please contact the Andrology Department 0114 2268349 (Monday to Friday 8am – 4pm) or sht-tr.AndrologyJessopFertility@nhs.net. We will explain what is involved and send you all the documents and information you need. We will take payment and and we will arrange a convenient day and time for you to attend.
How much will it cost for me to bank my sperm?
There is a one-off cost for pre-vasectomy sperm banking; it is not available on the NHS.
The cost includes the appointment, screening (for HIV, HTLV, and Hepatitis B and C), sperm freezing and 5 years’ storage. After 5 years if you would like to continue to store your sperm there will be a further charge, and so on. You will be expected to pay for your sperm banking in full before your appointment.
Please contact the Andrology Department 0114 2268349 (Monday to Friday 8am – 4pm) or sht-tr.AndrologyJessopFertility@nhs.net for current costs.
Will storing sperm guarantee my fertility in the future?
If you bank a good number of healthy sperm then there is a very high chance you will be able to use your stored sample for fertility treatment such as IVF or ICSI in the future. However, not all IVF cycles are successful, so even if you have good quality sperm stored, there is no guarantee the fertility treatment will work.
How much will treatment cost?
Costs for our most popular treatments are:
Intra Uterine Insemination (IUI)
including Ovulation Induction
£1000 per cycle (excluding drugs)
In Vitro Fertilisation (IVF)
including time lapse technology
£3300 per cycle (excluding drugs)
Donor Egg
excluding registration fee
£9200 per cycle
Competitive prices with no hidden extras
At Jessop Fertility, we take a transparent and simple approach to pricing, regardless of your circumstances.
When choosing a clinic it is important to compare costs. Some clinics may advertise low initial costs, but these prices often don’t cover the whole treatment costs. Our transparent pricing methodology ensures that you will not be faced with hidden extras and will receive the best quality service for the lowest cost. In addition, working within the NHS any profit from non NHS work is reinvested into the service for the benefit of staff and future patients.
Funding Options
Jessop Fertility offers treatment to patients who are eligible for NHS funding and those wishing to self-fund their treatment.
Eligibility to receive NHS Funded treatment will vary according to your Clinical Commissioning Group’s (CCG) criteria and your own personal circumstances.
If you are wishing to self-fund your treatment your GP will refer you to Jessop Fertility after undertaking the required preliminary fertility investigations.
We will do everything possible to help you become a parent
Over 3500 babies have been born as a result of treatment at Jessop Fertility
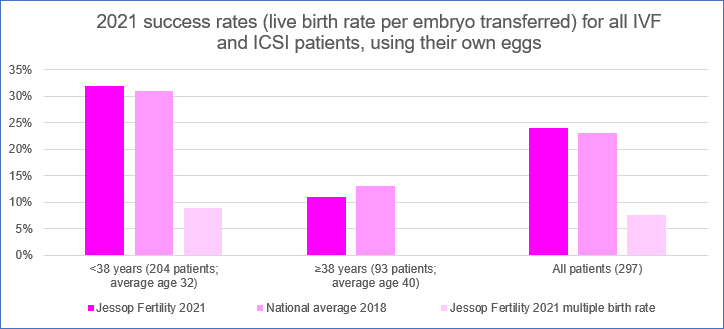
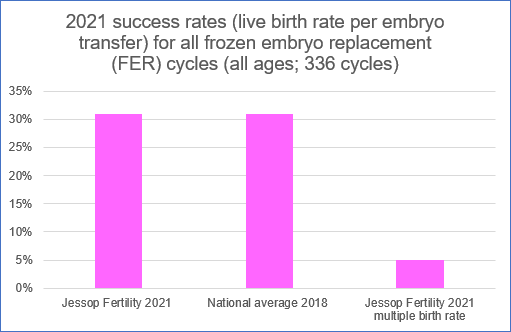
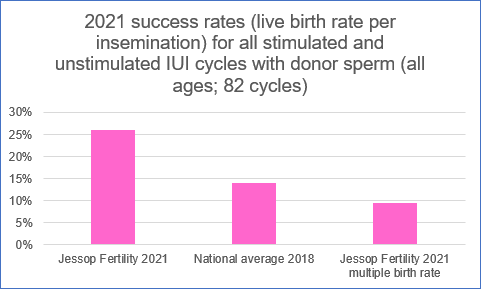
Our results
We are proud that our overall success rates for treating infertility consistently remain high. These charts show our latest live birth results (for 2021) compared with the national success rates published by the HFEA for 2018.
It is important to be mindful of the fact that success rates may vary for different people because of a variety of individual factors, which may increase or decrease the likelihood of you having a baby. Because of this, you should take into account other factors, in addition to information on success rates, when choosing your clinic. For more advice about choosing a clinic please visit the “Choose a Fertility Clinic” function on the HFEA website.
Feedback
If you’ve had treatment with us then please take the time to provide feedback to us and/or the HFEA using the links below. All feedback helps us to improve and deliver a high class service to every patient:
To leave feedback directly to Jessop Fertility please use Click Here.
If you would like to leave feedback about Jessop Fertility with the HFEA then please Click here.
Our Families' Stories
Shauna & Darrens Story
We were trying naturally for 9 years and in that time my husband had an op to reverse his vasectomy at a private hospital. We eventually raised enough money to have an egg share ivf/icsi cycle in September 2014. However sadly I only had 4 eggs collected from my right ovary as my left was being awkward and kept hiding so didn't have enough to share but went ahead with our cycle.
Samantha and Scotts Story
I’m Samantha, 28 & my partner is Scott, 30. We’re both from Batemoor Sheffield.We started our journey when I was 22 and Scott was 24 in September 2015 after the loss of his mum. We had been together for 6 years & knew we were ready to become parents… however my body decided differently.
Karrie & Adam’s Story
Karrie Sutton and her partner Adam Towey, both 38, are looking forward to what 2020 holds, not least celebrating their baby boy Elijah’s second birthday.
Starting the new decade as a family of three is a dream they once thought would never happen after trying for a baby for almost seven years.
Louise and Steve Willets’s Story
Louise, aged 36, from Dinnington, describes her journey towards welcoming her daughter through treatment at Jessop Fertility:
“After suffering from an aggressive form of MS, I was offered a stem cell transplant at Sheffield Teaching Hospital NHS Foundation Trust, which meant my immune system would be rebooted to halt the disease using chemotherapy.
Joanne and Robert Dowson’s Story
Joanne, aged 34, is a teaching assistant from Retford. She and her husband Robert welcomed baby boy Dexter George in January following IVF at Jessop Fertility.
Joanne said: “After three years of trying for a baby naturally, our IVF journey started in January 2016. To increase the chances of treatment working, I needed to lose a bit of weight. Although it wasn’t easy, I was so excited when I eventually reached my goal as it felt one step closer towards our dream of becoming parents.
Georgie and Marc’s Story
After four years of trying for a baby, Georgie and Marc Whitfield became the proud parents of Teddy (now 2) after receiving treatment at Jessop Fertility. Georgie from Nether Green, Sheffield, said: “Although our fertility journey has been the toughest period of my life, I would do it all again in a heartbeat. Being Teddy's mum is the most amazing privilege. He has brought us so much joy, happiness and love.”
Nicola and Jo’s Story
Globetrotting couple Nicola Minichiello and Jo Manning are the proud parents of seven month old twin boys, Zach and Freddie (born February 20th 2017), after having treatment at Jessop Fertility. Nicola who is from Renishaw in Sheffield, said: “We spent 4 years all together on our journey through infertility. After initially trying at home with a known donor for just over a year we suspected that maybe there was a reason I wasn’t getting pregnant. We were referred to have exploratory tests with Mr Skull at Jessop Fertility to determine if there were any issues.
Thank you to Nina for sharing her story!
"We started our journey with Jessop Fertility back in 2014 after trying to get pregnant to get pregnant for 3 years, we went through many tests and started our treatment in September 2014. It was an emotional rollercoaster, constantly worrying if each stage of the treatment would be successful, but we put our full trust into the team.
Huge thank you to Lindsay for sharing her wonderful story!
Lindsay, 37 who is a Financial Customer Advisor from Sheffield, gave birth to her baby girl Erin on the 24th of February 2019 following treatment from Jessop Fertility. "I started my journey with Jessops in March 2016, I was in a same sex relationship and having a child was something we had dreamed about for a long time. We had no clue where to start but after a referral from my GP our journey started. Due to an auto immune illness things were slightly more complicated for me
Thank you to Vicky and Richard for sharing their inspirational story…
Vicky, 31, who is a maths teacher in Huddersfield and her actor husband Richard, 42, welcomed their baby boy Lochlan in January 2018 following treatment at Jessop Fertility. Vicky said, “We first started trying for a baby eight years ago, after a few years we went to the doctors to run some tests and were told that we had severe male fertility problems and would need IVF.
How to start your journey
For both NHS Patients and Self-Funding Patients
A visit to your GP is all that is required.
Your GP will review you and your partner´s medical histories. They will discuss your general health and wellbeing and plan any preliminary investigations required.
You may require some routine blood tests to try and establish a diagnosis. If you have been diagnosed with sub-fertility by your GP or you suspect you might have fertility issues then Jessop Fertility is the right place for you.
Following referral by your GP you will usually be sent an appointment to attend the Fertility Clinic, held in Gynaecology out-patients which is based within the main Jessop Wing (Level One). During your medical consultation further investigations may be arranged. If you are unsure and require advice please contact the unit on Tel: 0114 226 8050 or use our...
Latest News
Robust tracing processes
It has been recently reported in the media (14 February 2024) about an issue affecting Guys Hospital and Jessop Fertility clinics. The issue related to a recall of a particular batch of a product used in the freezing of eggs and embryos process. We want to assure people using our services that we began a thorough patient review as soon as the product recall notice was issued by the supplier.

All About Fertility
All About Fertility is a great brand new resource for patients, providing articles, webinars and videos created by experts in the field of assisted reproduction. It also contains a support forum for all men who have questions about infertility, with plans to create a similar forum for women.

Jessop Fertility awarded top quality mark for patient care and satisfaction.
Jessop Fertility have once again received the ISO 2009:2015 standard accreditation for quality after passing an inspection from the International Organisation of Standards with flying colours.

Two new services at Jessop Fertility
We are excited to announce that we are now offering Fertility Health Checks and Social Egg Freezing.
There are many reasons why a man or women may experience difficulties when they decide the time is right to try for a family.

Jessop Fertility Open Afternoons
Jessop Fertility would like to invite you to one of our open afternoons in 2019 (3-5pm).
Come along to learn more about the treatments we offer, meet and chat with key members of the team and look around the unit.
7th December

Preimplantation Genetic Testing (PGT-A) now available at Jessop Fertility
Jessop Fertility now provides Preimplantation Genetic Testing (PGT-A) which allows our embryologists to identify embryos that have the correct number of chromosomes at a very early stage.
Jessop Fertility’s globe-trotting Embryologist shares good practice in Russia
Our Principal Embryologist, Rachel Cutting, was invited to Russia to give several lectures and practical teaching sessions to an enthusiastic group of embryologists at the Russian Society of Reproductive Medicine.
Couple welcome three babies against all odds thanks to innovate technology
A mum of three who feared she would never become a parent has praised fertility unit for offering time-lapse technology to all their patients at no extra cost.
Jessop Fertility celebrates 40 years of IVF
Jessop Fertility are celebrating the birth of the first ever IVF baby with a tea party for children who share the special birthday and were born as a result of their parents receiving treatment at the Unit.
Jessop Fertility involved in development of new "sperm radar" test
Jessop Fertility and scientists at the University of Sheffield have developed a new technique to examine human sperm without killing them - helping to improve the diagnosis of fertility problems.
Research
Jessop Fertility offers patients the chance to take part in research.
Research provides answers for healthcare workers so that we know what is the best care to give to our patients. During any research study patient safety is the most important factor to us as patient care and safety is at the heart of everything we do.
Below are the current research studies that are running at Jessop Fertility. If you would like more information please click the study logo and this will take you to the study websites.
HELP Fertility? – for people presenting with infertility or baby loss and fibroids or polyps. For more information please click here
STOP-OHSS Trial - STOP-OHSS: for people presenting with Ovarian HyperStimulation Syndrome. For more information please click here
DOMAIN – for people with low sperm counts
ULTRA – for people presenting with PCOS

Meet Our Team
Throughout your treatment you will be supported by our expert team of fertility specialists who will ensure you receive the best possible treatment and experience. Jessop Fertility employs a diverse range of people with a variety of skills and backgrounds. Meet our teams below to find out more.

Jonathan Skull is a Consultant in Reproductive Medicine and Surgery and the Clinical Head of Jessop Fertility. After graduating from Bristol University in 1988, he trained in Obstetrics and Gynaecology in Bristol, Sheffield and London. He was senior IVF co-ordinator at the Hammersmith Hospital working with Professor Lord Robert Winston. Upon returning to Sheffield in 1997, he then worked as a Clinical Lecturer at the University of Sheffield working with Professor Ian Cooke and Professor Bill Ledger.
He plays a key role in helping develop regional NHS fertility services. He is an expert adviser for the Specialised Commissioning Groups in Yorkshire and the Humber and the East Midlands.
Mr Skull has particular interests in laparoscopic and hysteroscopic surgery and tubal microsurgery, including reversal of sterilisation. He also has special interests in endometriosis, Polycystic Ovarian Syndrome (PCOS) and male factor infertility including surgical sperm recovery.
Ever thought of being a sperm donor?
You could help couples achieve their dream of having a family.
Donors will be financially compensated
Become a Sperm Donor
FAQs
Below are a number of questions/answers which you may find useful.
If you have any other queries which are not answered on this page please contact us.
Yes. There are several support groups for which we can give you contact details, depending upon your specific needs.
In addition you may want to have a look at the websites for the following organisations that may be able to offer you advice and support: The HFEA: www.hfea.gov.uk
National Gamete Donation Trust: www.ngdt.co.uk
Please always remember that our counselling service is also available to you. Please just ring reception on 0114 2268050 to speak to a counsellor or to make an appointment.
This needs to be discussed with your doctor/embryologist. Blastocyst transfer is where your embryos are grown to day 5 of development (day of egg collection is termed day 0). Using this technique allows us to gain more information about your embryos and how they are developing. Your doctor/embryologist will discuss whether or not you would be a suitable candidate for this. It is recommended if you are under 37 years of age and on your first or second cycle that you have a single blastocyst transferred during your IVF treatment. This is to avoid a multiple pregnancy but should still give you a good chance of a pregnancy. It is not suitable for all patients and requires a good number of eggs/embryos which are of good quality. At Jessop Fertility there is no extra charge for blastocyst culture. Whether you are self-funding or NHS-funded, all costs for this service are included in your treatment cycle.
If you have been sent an appointment to attend Andrology it will be so that we can check whether or not you have sperm in your ejaculate, how many there are and how well they are swimming. You will have been sent the appointment either because you would like to start a family (diagnostic semen analysis), or because you have had a vasectomy and we need to check if it has worked (post-vasectomy semen analysis).
Please click on the document below to find out more.
Diagnostic semen analysis Post vasectomy semen analysisAs part of your treatment you may have been given some progesterone pessaries. These help to keep the lining of your womb prepared for an embryo to implant. You can use your pessaries either vaginally or rectally, or a combination of both. If you use them vaginally then you may have some discharge. This is likely to be from the pessary coating and is nothing to worry about - just use a panty liner if you need to. There is usually very little discharge if you use the pessaries rectally, so you may find that this method is more convenient. We usually advise you to use the pessaries approximately 12 hours apart (e.g. 9 o'clock each morning and evening). However, on the day of your embryo transfer, please do not use your pessary that morning but bring it with you to use straight after your embryo transfer. You should keep using your pessaries until you attend for your pregnancy test. Depending on your pregnancy test result we will advise you whether or not you need to keep using them. If you have any other questions then please get in touch with the nurses.
All UK fertility clinics, both NHS and private, are charged a fee by the HFEA for each cycle of IVF, ICSI and donor insemination they carry out. This charge goes towards the costs of the clinic being regulated and inspected by the HFEA. Some clinics pass this fee on to their patients as an additional item on the bill. At Jessop Fertility, even if you are self funding your treatment, your HFEA fee is included in the cost of your cycle.
Yes there are female doctors in residence at the ACU and we will try to arrange that you see a female doctor for your treatment if this is what you wish. However, we are a busy clinic and it will depend upon which doctor is carrying out procedures that particular day, so we cannot guarnatee that there will be a female doctor available to see you. Please make your wishes known to our staff as soon as possible when you come for treatment.
Yes, we are always happy to talk to you if you are thinking about becoming a sperm or egg donor. To find out more, please have a look at our information for sperm donors and egg donors. Please contact us if you would like more information. There is no obligation at this stage, please feel free to just call us for an informal chat.
As you progress through your treatment cycle you may want to find out more about your embryos' development. Likewise, you may want to find out more about your options for thawing embryos for your frozen embryo replacement (FER) cycle, or to discuss your embryo quality and development after your cycle is complete. The Embryology Team are always happy to talk to you about these and other issues. Please contact reception on 0114 2268050 to arrange an embryology consultation if you think this would be helpful for you.
Yes, at Jessop Fertility we have 2 time lapse systems (Embryoscope™ and PrimoVision™) that can constantly monitor your embryos' development. Time lapse will benefit some patients more than others. If we feel that your chances might be helped by this technology then the embryologist will talk to you about it when you come in for your egg collection. If we think that you will benefit from time lapse, you won't be charged extra for it. The cost will be covered either by your NHS funding, or be included in the cost of your self-funded cycle. Find out more about time lapse here
We aim to provide the highest standards of care and are continually striving to improve our service to patients. Whilst we hope that you will be entirely happy with your treatment at the Jessop Fertility, we welcome any comments, suggestions or constructive criticism.
If you have a complaint about any aspect of your treatment, please do not hesitate to tell us and we will endeavour to resolve the matter immediately. You may complain either verbally, if the matter is not too serious, or in writing, addressing the complaint to Ms Val Kitcheman, Business Support Manager, if you feel that the nature of the complaint justifies a full investigation. If you would prefer to speak with someone outside of Jessop Fertility you can contact the Patient Advice and Liaison Service on 0114 271 2400 or email sth.pals@nhs.net.
All complaints and suggestions are recorded for monitoring purposes and may be inspected by the Human Fertilisation and Embryology Authority. We will respond quickly and sensitively to all written complaints, by acknowledging the complaint in writing. We will then investigate as necessary and respond in writing according to Trust policy. If you would like to meet to discuss the issue in greater detail we will be happy to arrange this. In some instances the matter cannot be dealt with satisfactorily within the specified time periods. If this is the case we will report regularly to you on the progress of the matter. If you do not believe that your complaint has been adequately dealt with, you may take the matter to the Chief Executive of the Sheffield Teaching Hospitals NHS Trust using the NHS complaints procedure or to the Human Fertilisation and Embryology Authority.
When you come in for your embryo transfer we will ask you to have a full bladder. The reason is that, for most women, a full bladder helps us to pass the catheter containing your embryo(s) more easily. It also may give us a clearer picture as we scan you during the transfer. We don't want you to be too uncomfortable for your embryo transfer, so don't make your bladder too full. It's actually more important that your bladder isn't empty, so just drink as normal but don't empty your bladder for an hour or two before your embryo transfer appointment. Don't be afraid to ask us for more advice if you're still unsure.
This can depend on many factors including your eligibility for funding and which treatment you need. We will do everything we can to ensure that you do not encounter any unneccessary delays to your treatment. Please contact us for more information.
You will have many different appointments before and as you come through for treatment. All vary in length depending on your personal circumstances and the type of treatment you are having. Below is a general guide:
Doctor's appointment (medical consultation): half an hour to an hour
Nurse appointment: half an hour to an hour and a half
Egg collection: Allow around 3 hours so that you have plenty of time to recover before heading home
Embryo transfer: Around half an hour
Intrauterine insemination (IUI): Around half an hour
Trial sperm prep: A couple of minutes for a chat, and then however long it takes you to produce a semen sample
If you have 3 or more good quality embryos on day 3 then we may suggest that we continue to grow them in the lab until day 5. At this point we would hope that some of your embryos may have formed blastocysts. We will talk to you every day whilst your embryos are growing in the lab. We will make the decision with you about whether or not to grow your embryos to the blastocyst stage. This decision won't be made until we know how many embryos you have made and what their quality is like. You will both be involved in making this decision. It is not unusual to have only one or two blastocysts on day 5, even if you have several good quality embryos on day 3. In some cases the embryos might not form blastocysts at all. However, by growing them until day 5 we will know which of your embryos are the strongest and the most likely to form a successful pregnancy. It is incredibly rare for all embryos to stop developing on day 3.
This depends upon several factors: your age; embryo quality; whether or not you have been pregnant before; and how many treatments you have had previously. Our general recommendations are if you are aged 37 and under, on your first cycle and have good quality embryos you should replace one embryo in your IVF cycle (we may be able to freeze some of the remaining embryos). This is because there is only a very small difference between the pregnancy chances when replacing one or two embryos in this group of patients, but the chance of a twin pregnancy is much higher. There may be circumstances under which we may discuss with you the possibility of having two embryos replaced. If you are younger than 40 then by law you are allowed a maximum of two embryos to be replaced, although some health authorities will stipulate a single embryo transfer in the funding contract.
In orer to maximise the chances of conception and to help pregnancy outcome, you should consider the following aspects of preconceptual care: Folic acid: This has been shown to reduce the occurence of Spina Bifida. You should take 400 micrograms daily for 4 months before conception and continue until the 12th week of pregnancy. Rubella: You should check your immunity to Rubella (german measles) through your GP. Cervical smear: You should be up to date with your cervical smears. Weight: You should try and make sure your weight is within the normal limits. NHS funding can be affected if you very over- or under-weight. Limiting your alcohol intake and stopping smoking may increase your chances of pregnancy and general health and wellbeing.
At Jessop Fertility we offer a "package" price for your treatment cycle. We have no registration fees and no hidden charges. The package price includes: HFEA fee (where appropriate) cycle monitoring HIV screening counselling early pregnancy monitoring blastocyst culture time lapse culture (if recommended) It does not include: Consultations fees drug costs any non-routine investigations embryo freezing and storage anaesthetic costs for patients who prefer to have general anaesthetic for their egg collection extra unforeseen procedures that are necessary for your treatment (such as ICSI or surgical sperm retrieval) Before you start your treatment cycle we will provide you with your personalised "costed treatment plan" which will outline exactly what you will pay for your cycle. Please have a look at our costs for more information.
Side effects may occur from the fertility drugs taken during your cycle. These may include hot flushes, feelings of depression or irritability, headaches and restlessness.
One of the major risks of fertility drugs is ovarian hyper-stimulation syndrome (OHSS). OHSS is a result of sensitivity to the fertility drugs and the development of many eggs in the ovary which can become large and painful. Symptoms of mild OHSS include abdominal pain and bloating, nausea and vomiting. Occasionally cases of severe OHSS are observed which are associated with an increase in vascular permeability and the build up of fluid in the body resulting in cardiac, respiratory and renal problems. Our treatments aim to greatly reduce your risk of developing OHSS.
There is a slightly higher risk of ectopic pregnancy with IVF, by which a fertilised egg implants in the fallopian tube rather than the womb.
Multiple births are one of the major risks of IVF and the incidence of double (twins) or triple (triplets) gestations is increased with treatment. While for many couples struggling to have children this may seem like a bonus, multiple pregnancies carry many serious medical risks to both the mother and the babies:
Multiple gestations can: cause your blood pressure to rise significantly; increase your risk of developing diabetes and increase the risk of a still birth. Approximately 50% of twins and 90% of triplets are born premature or at a low birth weight. It is approximately 5 or 9 times more likely (for twins and triplets respectively) that a multiple birth baby will not survive the first week of life over that of a singleton baby. Also, babies from multiple gestations display an increased occurrence of cardiac defects.
To reduce the risk of multiple births there are strict guidelines regarding the number of embryos a woman can have transferred back. The governing body for IVF treatment in the UK, the Human Fertilisation and Embryology Authority (HFEA), insists that a maximum of two embryos are put back into the womb during treatment in women under the age of 40. The HFEA also encourages elective single embryo transfer (eSET) in women who are most at risk of having twins such as women 37 years or under who have a good number of quality embryos. At Jessop Fertility we suggest eSET for women under 37 years of age who have a good number of quality embryos at the day5/blastocyst stage.
We are open Monday to Friday 8.00am - 5.00pm and from 8.00am to 3.30pm on Saturdays. We also have 24 hour emergency nursing cover during your treatment. You will be given information on how to access this service once you start your treatment cycle.
Once you have had your embryo transfer you can carry on as normal. However we do advise you to follow these lifestyle guidelines: Avoid any foods that are not recommended for pregnant women, such as unpasteurised dairy products. Do not smoke or drink alcohol. There is no need to stop exercising if this is something that your body is used to. However, do not do too much and become over-tired. You are fine to return to work, assuming you have recovered well after your egg collection. If you have a job that involves strenuous physical activity then please ask for individual advice. You are fine to continue to have sexual intercourse. Continue with your pessaries or other medication until we tell you otherwise. If you have any doubts or queries then please contact us and speak to one of our nurses.
ICSI is a technique where a single sperm is injected into each egg during the IVF process. ICSI is recommended where the male partner has a low sperm count or the number of sperm swimming (motility) is low or if you have had a previous cycle of treatment where none or a very low number of eggs have fertilised. All of the other steps in the IVF process are the same.
This depends what results you are ringing for. Pregnancy results are available from 1:30-2pm. All other results are available from 2-3:30pm. The number you need to ring for all results is 0114 2268066
Parking can be a problem around the Jessop Wing/Hallamshire Hospital. There is a pay and display car park at the Jessop Wing but you may struggle to find a space as numbers are limited. There is a large multi-storey car park at the main Royal Hallamshire Hospital which is well signed. However, this car park also fills up by about 1030 each day, with spaces then becoming avaialable as and when people leave. In April 2016 a new public multi-storey car park opened on Durham Rd, opposite the Children's Hospital, which is just a few minutes walk from the Jessop Wing. There is limited street parking, often with time restrictions. There are some public car parks in Broomhill which is a 5-10 minute walk away. If you are travelling by car then we would advise allowing plenty of time to find a parking space.
As you come through for your IVF or ICSI cycle we will talk to you about how your embryos are likely to develop from day 1 to day 5 or 6.
Day 0 is the day of your egg collection.
Day 1 is the day that we check for fertilisation.
Day 2: we expect your embryos to have 2-4 cells.
Day 3: we expect your embryos to have 5-8 cells.
Day 4: we do not look at your embryos as they are difficult to grade and assess at this stage (morula stage).
Day 5: we hope that your embryos may have developed into one or more blastocysts.
The vast majority of eggs that fertilise on day 1 (the day after your egg collection) will usually go on and form an embryo on day 2. Therefore, if you have a reasonable number of eggs that have fertilised (usually 3 or more) then we will not ring you on day 2. However, if your day 2 falls on a Saturday, meaning that you would not be able to have a day 3 transfer (on Sunday) then we may ring you on day 2. On day 4 of development (4 days after your egg collection) your embryos should be at the "morula" stage. A morula is a ball of cells that are usually too many to count. It is also difficult to assess the quality of the cells, even if we are able to count them. Because it is so difficult to grade your embryos at this stage, we won't usually look at them on day 4 and we won't ring you. You will be told a day and time for your embryo transfer when we speak to you on day 3.
This will depend upon a number of criteria and you will need to ask your GP/ clinic administration department to find out if your treatment is covered. The criteria are different for each primary care trust.
If you want or need to self fund please see our costs.
If you have any queries regarding your funding then please contact us.
Contact us
We’d love to answer any questions you may have. If you would like find out more please complete our contact form or send an email to sth.jessopfertilityadministration@nhs.net
Alternatively you can call us on: 0114 226 8050
Opening times:
Monday to Friday: 8.00am - 5.00pm
Saturday: 8.00am - 3.30pm
Results Line:
0114 2268066
Monday-Saturday 2.00pm - 3.30pm
The Jessop Wing
Tree Root Walk, Sheffield S10 2SF